Editor's note: Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.
Primary care practices stand to lose almost $68,000 per full-time physician this year as COVID-19 causes care delays and cancelations, researchers estimate. And while some outpatient care has started to rebound to near baseline appointment levels, other ambulatory specialties remain dramatically down from pre-pandemic rates.
For primary care practices, Sanjay Basu, MD, and colleagues calculate the losses at $67,774 in gross revenue per physician (interquartile range [IQR], $80,577 - $54,990), with a national toll of $15.1 billion this year.
That's without a potential second wave of COVID-19, note Basu, director of research and population health at Collective Health in San Francisco, California, and colleagues.
When they add a theoretical stay-at-home order for November and December, the estimated loss climbs to $85,666 in gross revenue per full-time physician, with a loss of $19.1 billion nationally. The findings were published online June 25 in Health Affairs.
Meanwhile, clinical losses from canceled outpatient care are piling up as well, according to a study by Ateev Mehrotra, MD, associate professor of health care policy and medicine at Harvard Medical School in Boston, Massachusetts, and colleagues, which calculates the clinical losses in outpatient care.
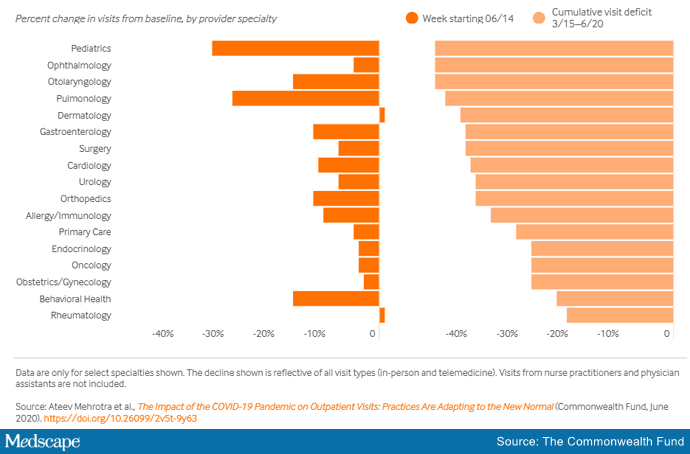
"The 'cumulative deficit' in visits over the last 3 months (March 15 to June 20) is nearly 40%," the authors write. They reported their findings in an article published online June 25 by the Commonwealth Fund.
When examined by specialty, Mehrotra and colleagues found that appointment rebound rates have been uneven. Whereas dermatology and rheumatology visits have already recovered, a couple of specialties have cumulative deficits that are particularly concerning, Mehrotra told Medscape Medical News. For example, pediatric visits are down by 47% in the 3 months since March 15 and pulmonology visits are down 45% in that time.
Much Depends on the Future of Telehealth
Closing the financial and care gaps will depend largely on changing payment models for outpatient care and assuring adequate and enduring reimbursement for telehealth, according to experts.
COVID-19 has put a spotlight on the fragility of a fee-for-service system that depends on inperson visits for stability, Daniel Horn, MD, director of population health and quality at Massachusetts General Hospital in Boston, told Medscape Medical News.
Several things need to happen to change the outlook for outpatient care, he said.
A need mentioned in both studies is that the COVID-19 waivers that make it possible for telehealth visits to be reimbursed like other visits must continue after the pandemic. Those assurances are critical as practices decide whether to invest in telemedicine.
If US practices revert as of October 1, 2020, to the pre-COVID-19 payment system for telehealth, national losses for the year would be more than double the current estimates.
"Given the number of active primary care physicians (N = 223,125), we estimated that the cost would be $38.7 billion (IQR, $31.1 billion - $48.3 billion) at a national level to neutralize the gross revenue losses caused by COVID-19 among primary care practices, without subjecting staff to furloughs," Basu and colleagues write.
In addition to stabilizing telehealth payment models, another need to improve the outlook for outpatient care is more effective communication that inperson care is safe again in regions with protocols in place, Horn said.
However, the most important change, Horn said, is a switch to prospective lump-sum payments — payments made in advance to physicians to treat each patient in the way they and the patient deem best with the most appropriate appointment type — whether by inperson visit, phone call, text reminders, or video session.
Prospective payments would take multipayer coalitions working in conjunction with leadership on the federal level from the Centers for Medicare & Medicaid Services, Horn said. Commercial payers and states (through Medicaid funds) should already have that money available with the cancelations of nonessential procedures, he said.
"We expect ongoing turbulent times, so having a prospective payment could unleash the capacity for primary care practices to be creative in the way they care for their patients," Horn said.
Visit Trends Still Down
Calculations by Basu, who is also on the faculty at Harvard Medical School's Center for Primary Care, and colleagues were partially informed by Mehrotra's data on how many visits have been lost because of COVID-19.
Mehrotra said a clear message in their study is that "visit trends are not back to baseline."
They found that the number of visits to ambulatory practices had dropped nearly 60% by early April. Since then, numbers have rebounded substantially. As of the week of June 14, overall visits compared to baseline were down 11%. But the drops varied widely across specialties.
Mehrotra said he found particularly disturbing the drop in pediatric visits and the sharp contrast between those rates and the higher number of visits for adults.
While visits for patients aged 75 and older had climbed back to just 3% below baseline, the drop seen among kids aged 3-5 years remains 43% below baseline.
"Even kids 0-2 years old are still down 30% from baseline," he pointed out.
It's possible that kids are getting care from other sources or perhaps are not sick as often because they are not in school, he said.
However, he added, "I do think there's a concern that some kids are not getting the care they need for chronic illnesses such as attention deficit hyperactivity disorder, asthma, eczema, and psoriasis, and vaccination rates have fallen."
Telemedicine Rates Dropping
Telemedicine was "supposed to have its shining moment," Mehrotra said, but trends show it cannot make up the gaps of inperson care.
His team's data show a decline in telemedicine as a percentage of all visits from a high of 13.8% in mid-April to 7.4% the week of June 14.
He attributes that partially to physicians' mixed success in getting reimbursed.
"While Medicare has done a good job reimbursing, commercial payers and Medicaid plans have been mixed in their coverage," he said.
Some physicians who don't get reimbursed or receive delayed or reduced payments are going back to inperson visits, Mehrotra said.
He said it's important to remember, though, that before the pandemic, "telemedicine was making up 0.1% of all visits."
"Even if now it declines (from the April high of 13.8%) to 5% or 3%, that's still a 30-fold increase within the course of a couple of months," he pointed out.
Prospective payments would help expand the possibilities for telemedicine, he said, and could include apps and wearables and texts in addition to or instead of traditional video sessions.
Mehrotra said change won't come fast enough for some and many practices won't survive.
"People are worried about their livelihood. This is nothing we've ever — at least in my career as a physician — had to focus on. Now we're really having practices ask whether they can financially sustain themselves."
For many, he said, the damage will be long term.
"That cumulative deficit in visits — I'm not sure if it's ever coming back," he said. "If you're a primary care practice, you can only work so hard."
Basu has reported receiving a salary for clinical duties from HealthRIGHT360, a Federally Qualified Health Center, and Collective Health, a care management organization. Horn and Mehrotra have reported no relevant financial relationships.
Health Affairs. Published online June 25, 2020. Full text
The Commonwealth Fund, 2020. Report
Marcia Frellick is a freelance journalist based in Chicago. She has previously written for the Chicago Tribune and Nurse.com and was an editor at the Chicago Sun-Times, the Cincinnati Enquirer, and the St. Cloud (Minnesota) Times. Follow her on Twitter at @mfrellick
Follow Medscape on Facebook, Twitter, Instagram, and YouTube.
"lose" - Google News
July 02, 2020 at 08:21PM
https://ift.tt/2NOwqwL
PCP Practices May Lose About $68K Per Physician This Year - Medscape
"lose" - Google News
https://ift.tt/3fa3ADu https://ift.tt/2VWImBB
Bagikan Berita Ini














0 Response to "PCP Practices May Lose About $68K Per Physician This Year - Medscape"
Post a Comment